More Than a Measurement: COPD
When you are diagnosed with Chronic Obstructive Pulmonary Disease (COPD), you may be instructed to monitor your health parameters at home, possibly including your blood pressure and weight. You may begin to feel your life is being ruled by numbers: the numbers on the screens of your blood pressure monitor and scale.
At A&D Medical, we understand that these measurements are just a small part of who you are. To ensure your health, you must monitor and manage your weight and blood pressure. But the good news is that as you do, you’ll be empowered to make decision that can improve the bigger parts of your life – the parts that matter most to you.
What is COPD?
A progressive, inflammatory lung disease, COPD is most commonly associated with symptoms such as difficulty breathing, excessive coughing, and wheezing which may get worse over time. According to the American Lung Association, more than 11 million people have been diagnosed with the condition, and it is the third leading cause of death in the United States.
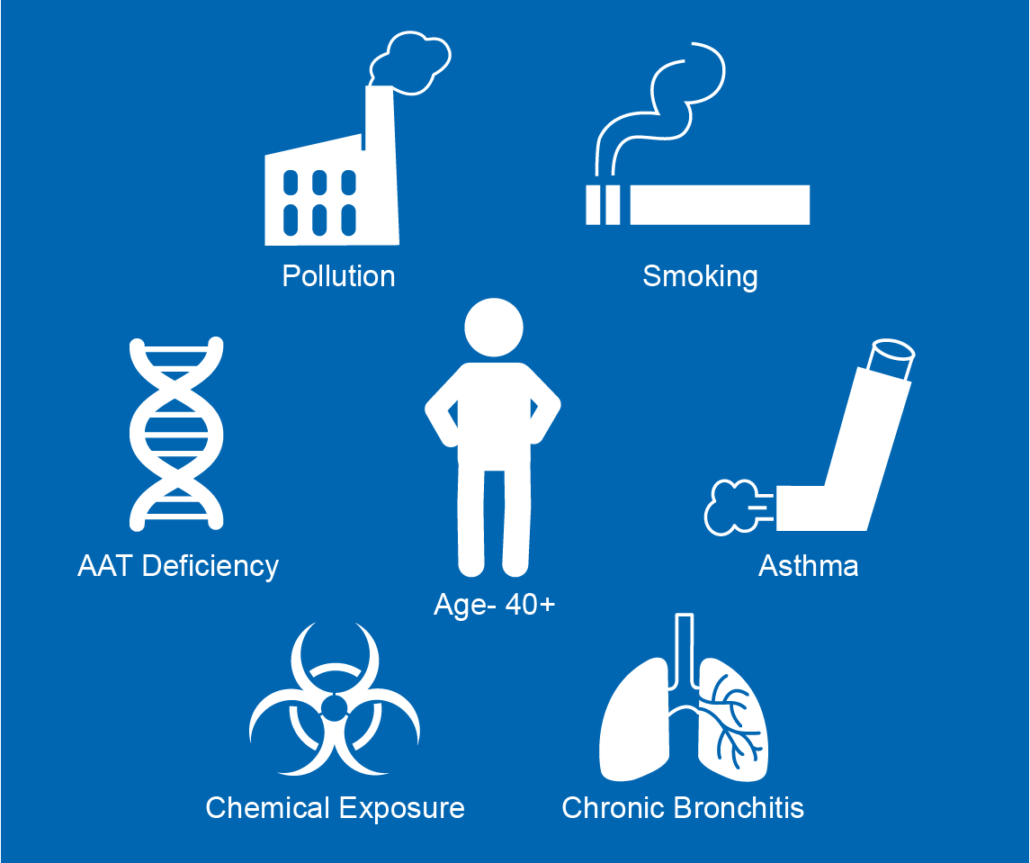
Its origins can be anything from exposure to cigarette smoke or other irritants to chronic bronchitis or emphysema.
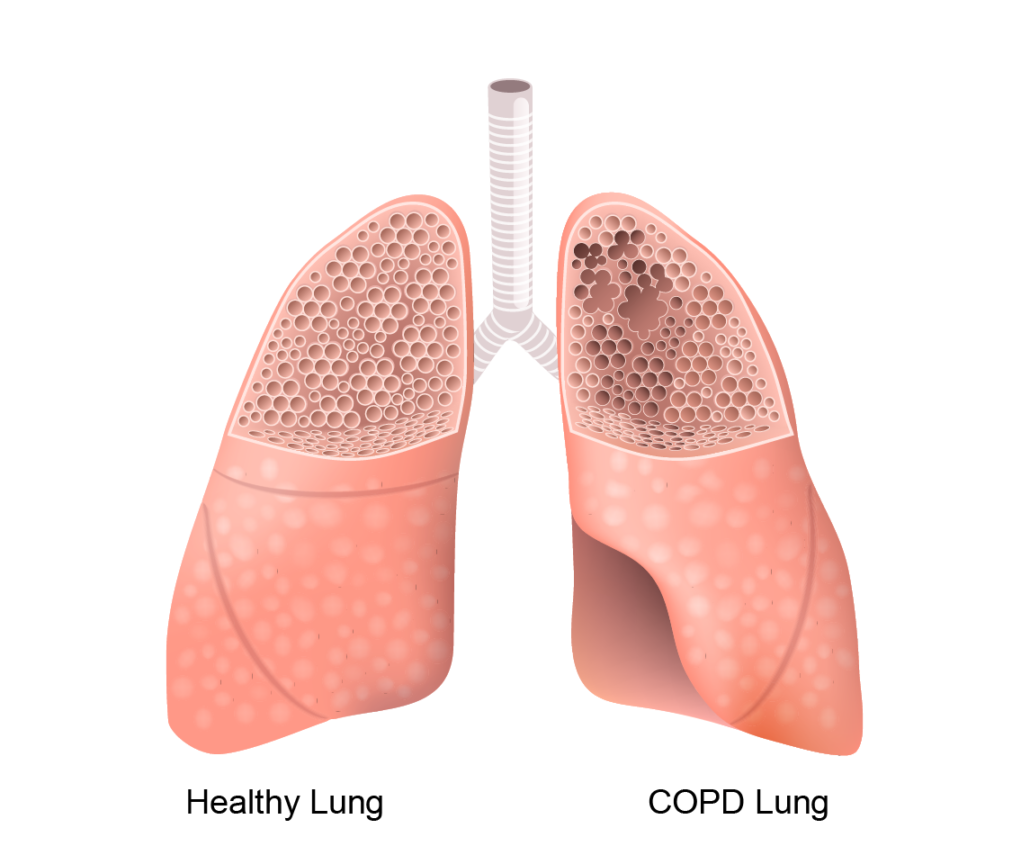
Regardless of how you came to have COPD, the bronchioles (the small tubes with air sacs or alveoli at the ends) in your lungs have been damaged, but the good news is that it can often be controlled by reducing exposure to irritants or by making lifestyle changes.
What’s important to know about COPD?
There are many risk factors that lead to COPD, such as exposure to tobacco smoke, fumes, chemicals, and other irritants, as well as asthma, age, and even family history. If you have any of the risk factors and experience symptoms such as shortness of breath, wheezing, a chronic cough, tightness in your chest, low energy, or swelling in your lower extremities, you should make an appointment with your doctor.
In addition to the daily struggles you might face with COPD, other complications may arise as well. Because of how your lungs are affected, respiratory infections may be more likely, as is your risk for heart disease, lung cancer, and more.
Because COPD is often a preventable disease, the best path is to avoid irritants – or if you have been a long-term smoker, talk to your doctor about getting help quitting.
How does COPD affect most people?
When someone has COPD, the bronchioles in their lungs are damaged, and their bronchiole tubes may have thickening or inflammation as well as a loss of elasticity.
On top of the physical changes to the lungs themselves, many people experience an increase in mucus, which can obstruct breathing.
The combination of these factors means that less air can get in and out of your lungs, which makes you feel short of breath and tired. You may also frequently cough or wheeze due to excess mucus, and you may find that you experience respiratory infections more often than your friends and family.
The American Lung Association recommends getting checked out if you have questions or concerns about whether you might have COPD. “COPD is often not found until the disease is very advanced because people do not know the early warning signs. Sometimes people think they are short of breath or [can’t] take part in their normal activities because they are ‘just getting older.’” In the case of COPD, though, prevention can make a huge difference in the severity or treatment of your case.
What other health conditions play a role in COPD?
Like many other chronic conditions, once you have one, you may find yourself at risk for others. Unfortunately, COPD is no different. Many other conditions may need to be monitored once you are diagnosed with COPD, including:
- Obesity
- Pulmonary hypertension
- Heart disease
- Diabetes – approximately 15% of people with COPD also have diabetes.
- Gastroesophageal reflux disease (GERD)
- Sleep disorders
Why does monitoring your blood pressure help you control COPD?
COPD, as noted above, can have relationships with a variety of serious conditions, including hypertension and other forms of heart disease.
Hypertension is another name for high blood pressure, so if your doctor has prescribed home blood pressure monitoring after your COPD diagnosis, it makes sense! Your doctor likely knows that COPD is linked to an increased risk of serious heart-related conditions, such as heart attack, irregular heartbeats, blood clots, and more. In fact, you may even be asked to wear an ambulatory blood pressure monitor, also known as a 24-hour blood pressure monitor.
When you monitor your blood pressure at home, using a standard home monitor or a prescribed ambulatory monitor, you are providing your doctor with important data about the stress and influences your body is experiencing. This can help them adjust your treatment plan or provide early intervention in case of an emergent situation.
Why does monitoring your weight help you control COPD?
COPD is often linked with both diabetes and obesity, and body weight can be a critical component for all three conditions. Much like monitoring your blood pressure, monitoring your weight can help your doctor make informed decisions about the progress of your treatment.
After a COPD diagnosis, you may be asked to monitor your weight, or even adjust your weight with lifestyle and diet changes. In some cases, weight loss may be required, and in others, your doctor may request that you gain weight.
With a Bluetooth scale like this one, you can take your weight and send your results to your doctor from the A&D Connect app. Communication like this helps your doctor understand your progress in real time without having to make an appointment.
What else can you do to control COPD?
The first thing your doctor will likely tell you do to help control COPD if you’re a smoker is to quit smoking. Easier said than done, we know, but your doctor can walk you through a number of options that might be helpful, from nicotine replacements to various forms of counseling.
After that, your doctor is likely to tell you to take care of yourself. That means eating a healthy, balanced diet of frequent, small meals, getting regular exercise, and plenty of rest. If prescribed, you will also be asked to comply with your prescription and oxygen therapy, both of which can help prevent and control issues.
Additionally, you may given other advice, such as learning breathing techniques or getting vaccinations to prevent lung infections.
Can home blood pressure monitors detect pulmonary hypertension?
Unfortunately not. A&D Medical blood pressure monitors are designed to measure the blood pressure in your heart’s arteries, but pulmonary hypertension is the blood pressure in your lungs’ arteries. To diagnose pulmonary hypertension, you may be given a CT scan, an MRI, a pulmonary function test, etc. If pulmonary hypertension is a concern for you, please speak with your doctor.
Can hypertension cause COPD?
While hypertension and COPD are related conditions, hypertension does not cause COPD. If you have COPD and hypertension, you may be asked to make lifestyle and diet changes to manage your hypertension, which may also help your COPD symptoms improve.
What are the stages of COPD?
As with hypertension, there are multiple stages of COPD. The stages are often explained in terms of a forced expiratory volume test (FEV1), which determines how much air you can exhale over one second.
- Stage 1 / Very Mild COPD: FEV1 scores >80% of a healthy person’s scores
- Stage 2 / Moderate COPD: FEV1 scores between 50%-80% of a healthy person’s scores
- Stage 3 / Severe COPD: FEV1 scores between 30%-50% of a healthy person’s scores
- Stage 4 / Very Severe COPD: FEV1 scores <30% of a healthy person’s scores
Is COPD the same as asthma?
No, although many people may mistake the symptoms for one another. In fact, the two conditions are very different, even if they are both commonly associated with a shortness of breath and wheezing. People with either disease have trouble breathing due to changes to the structure and function of your airways, combined with excess mucus.
Asthmatics often experience these symptoms after an environmental trigger. On the other hand, people with COPD experience these symptoms without needing to be exposed to a trigger, but when there is a trigger, the symptoms can worsen dramatically.
Is COPD the same as emphysema?
In some cases, yes, emphysema and COPD are the same. COPD, however, is a group of lung diseases, but it is not always emphysema. Emphysema is when the walls of the air sacs at the end of the bronchioles are destroyed. This makes it harder for old air to be expelled, and it also makes it harder for new, fresh air to enter the bloodstream.
Don’t see your question? See our full list of FAQs.